Epilepsy in Canada: Prevalence and impact
Epilepsy is a neurological condition that affects almost 140,000 Canadians, according to data gathered by Statistics Canada. The disorder is characterized by seizures, which range from relatively mild (a moment of impaired concentration) to extreme (total loss of consciousness and awareness). Cannabis based medicines – and CBD-dominant products in particular – have proven to be very effective at reducing the frequency and severity of epilepsy seizures. With that said, medical cannabis should only be used in treatment resistant cases of seizures.
Abstract
Tables and Figures
Epilepsy is a chronic neurological condition characterized by spontaneous seizures, ranging in severity from a lapse in concentration to unconsciousness. The World Health Organization recognizes epilepsy as a major public health concern, estimating that more than 50 million people worldwide live with the condition. Epilepsy may be genetic in origin or the result of conditions affecting the brain such as tumors, infection, head injury, lack of oxygen (for example, at birth), and stroke. However, in more than half of cases, the cause is unknown. Epilepsy can be diagnosed at any age, and is associated with increased risk of premature death. An estimated 65% to 85% of cases eventually enter long-term remission.
This study examines the prevalence of epilepsy in Canada among people in long-term care facilities, based on the Survey of Neurological Conditions in Institutions in Canada, and among residents of private households, based on the Canadian Community Health Survey Neurological Conditions Prevalence File (see The data). In-depth information from the Survey on Living with Neurological Conditions in Canada is presented for household residents aged 15 or older: age at diagnosis and years since diagnosis, comorbid conditions, medications, and impacts, such as on education and employment.
The study pertains to people with “active” epilepsy; that is, those diagnosed with epilepsy who had had a seizure within the past five years or were currently taking antiepileptic medication. For context, the prevalence of comorbid conditions among this group is compared with the general household population.
Prevalence
Based on data for the 2010-to-2012 period, an estimated 139,200 Canadians had epilepsy―10,600 in long-term care facilities and 128,600 in private households (Table 1).
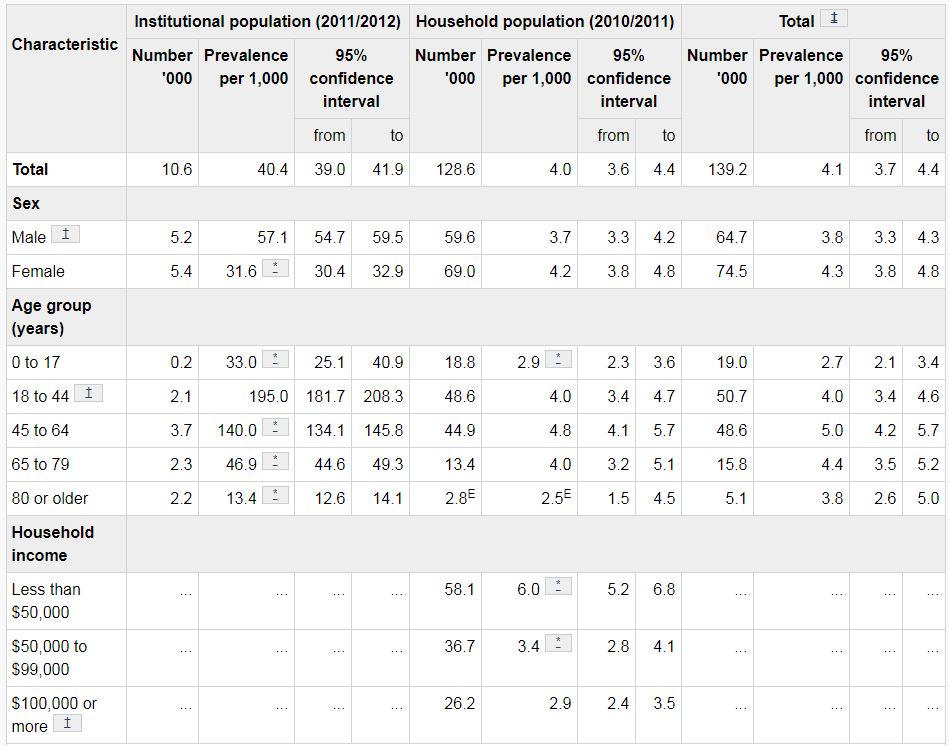
Table 1
Number with epilepsy and prevalence per 1,000, by selected characteristics, institutional and household population, Canada excluding territories, 2010 to 2012.
Among people in long-term care facilities, the overall prevalence of epilepsy was 40.4 per 1,000. The figure rose from 33.0 per 1,000 among children and youth to a peak of 195.0 per 1,000 at ages 18 to 44, and then dropped with advancing age. Males were more likely than females to have epilepsy: 57.1 versus 31.6 per 1,000.
In private households, no difference in prevalence was apparent between the sexes. The overall prevalence―4.0 per 1,000―was somewhat lower than estimates from other Canadian household surveys (5.2 to 5.9), which may reflect the stricter inclusion criterion of “active” epilepsy in the present study. In the household population, children and youth were less likely to have epilepsy (2.9 per 1,000) than were 18- to 44-year-olds (4.0 per 1,000). Prevalence was not significantly different at age 45 or older, compared with ages 18 to 44.
People in lower income households were significantly more likely to have epilepsy than were those whose annual household income was $100,000 or more, an inverse association consistent with previous studies. This may be due to a socioeconomic gradient in health and exposure to risk factors, or reflect the impact epilepsy can have on educational and occupational opportunities.
Age at diagnosis
About a quarter (26%) of household residents with epilepsy had been diagnosed before age 10; 75%, before age 30 (Figure 1). Another 15% had been diagnosed in their 40s or later. On average, people with epilepsy had lived with the condition for 24 years, although the period ranged up to more than 60 years.
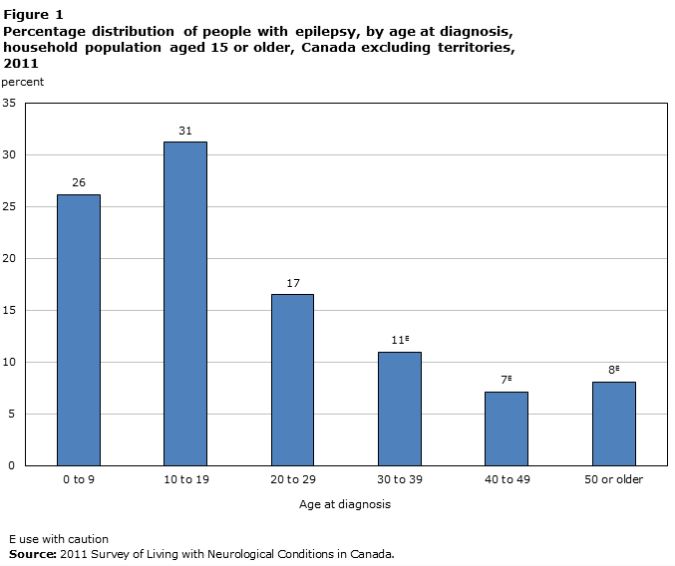
Figure 1
Percentage distribution of people with epilepsy, by age at diagnosis, household population aged 15 or older, Canada excluding territories, 2011.
Comorbidity
For close to two-thirds (64%) of household residents with epilepsy, it was their only neurological condition (Figure 2). Among those with another neurological condition, migraine was reported most frequently, followed by brain injury and stroke.
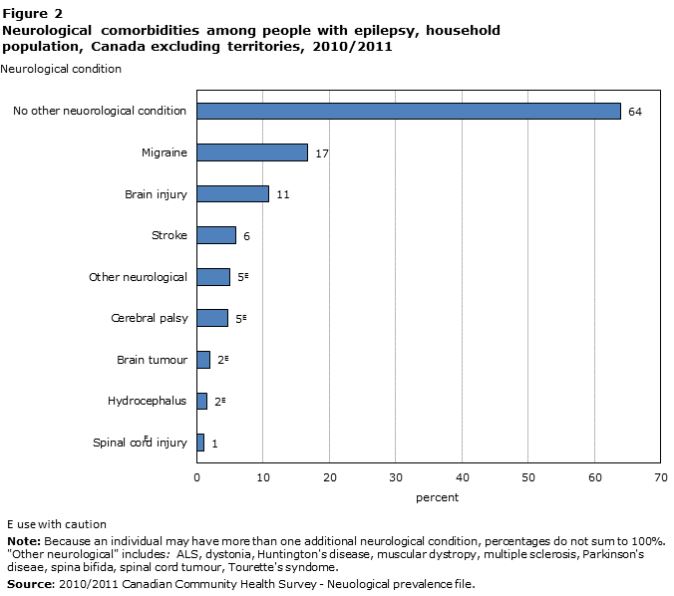
Figure 2
Neurological comorbidities among people with epilepsy, household population, Canada excluding territories, 2010/2011
The presence of additional chronic conditions can have important implications for quality of life and the need for health care services (Figure 3). People with epilepsy were about eight times more likely than the general population to report incontinence (34% versus 4%), which may be related to the effects of seizures on autonomic function. By contrast, the prevalence of diabetes, heart disease, and high blood pressure did not differ significantly from the general population.
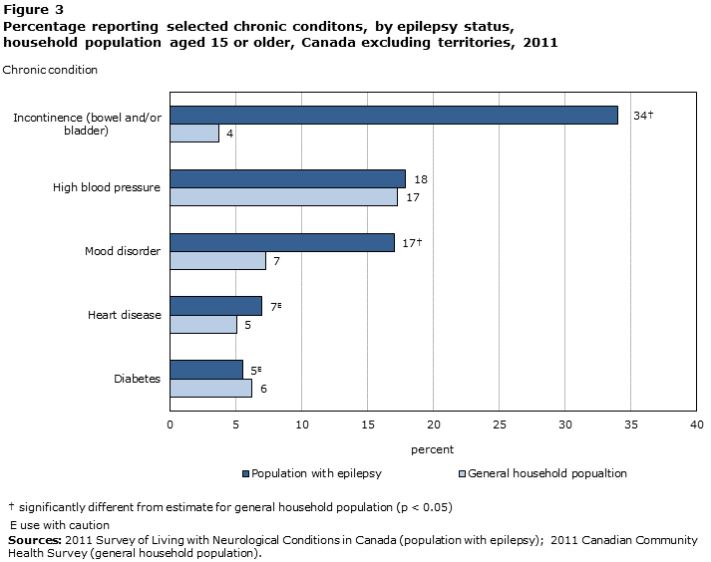
Figure 3
Percentage reporting selected chronic conditions, by epilepsy status, household population aged 15 or older, Canada excluding territories, 2011.
Those with epilepsy were more than twice as likely as the general population to have a mood disorder (17% versus 7%). Research has found that while people with epilepsy are at increased risk for psychiatric disorders, those with psychiatric disorders are also at increased risk of developing epilepsy.
Medication
Although surgery is an option, medication to control seizures is the primary treatment and is effective in about 70% of cases.
A third (34%E) of household residents whose only neurological condition was epilepsy and who were taking related medication had paid at least $500 out of pocket for these drugs in the past 12 months. Just under a third (29%E) reported side effects from the epilepsy drugs; for 61%E of them, the side effects had a moderate-to-extreme impact on their life.
Compared with when they had first been diagnosed, 56% people with epilepsy reported feeling much better, 27% somewhat better, and 17% the same or worse. Those who felt better credited this to medication (90%), coping strategies (10%), and/or surgery (4%).
Impact
The impact on quality of life varies among individuals. For example, 39% of household residents with epilepsy and no other neurological condition reported that it did not affect their life at all. An estimated 44% said that their life was affected a little bit or moderately, and the remaining 18% felt that epilepsy affected their life quite a bit or extremely (Table 2).
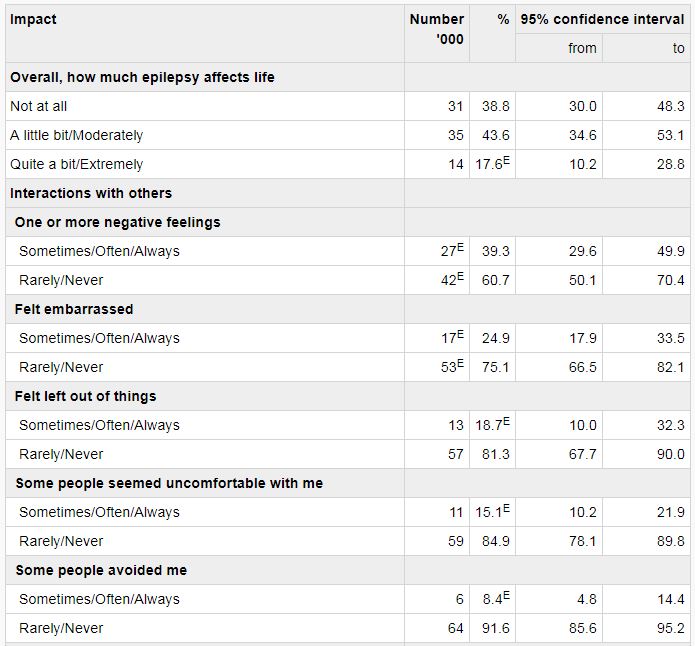
Table 2
Number and percentage with epilepsy, by effect on life and extent of limitations, household population aged 15 or older, Canada excluding territories, 2011.
For some, the stigma related to epilepsy is a considerable challenge. In this study, 39% reported negative feelings about their interactions with others because of their condition, including feeling embarrassed (25%) that they were left out of things (19%) or that people were uncomfortable with them (15%) or avoided them (8%).
Among the 44% with a valid driver’s license, 64% stated that they had been prevented from driving on occasion because of epilepsy. Of those without a driver’s license, 61% said that this was due to the condition.
For 29% of household residents with epilepsy, it interfered with their ability to get a good night’s sleep.
While two-thirds (67%) reported that epilepsy did not limit their educational opportunities, 25% reported some limitations, and 9% reported that the limitations were more extreme.
Epilepsy also affected employment opportunities: 21% felt limited a little bit or moderately, and 23% reported that they were limited quite a bit or extremely. Half of household residents with epilepsy were employed; 40% did not have a job; and the remaining 9% were permanently unable to work (Table 2). Among those not working, 19% reported that this was because of epilepsy. A similar percentage (19%) cited another illness, condition or disability; 26%, retirement; and 37%, other circumstances such school attendance, family responsibilities, and unemployment.
Of those not working, 79% said that they had had epilepsy when they worked in the past, and 27% had made changes as a result of the condition, such as reducing the number of hours, changing the type of work, or stopping work altogether.
Conclusion
In the 2010-to-2012 period, an estimated 139,200 Canadians reported having epilepsy. Epilepsy was diagnosed across the life course, but usually before age 30 (75%). For the majority (64%), epilepsy was their only neurological condition. Compared with the general population, people with epilepsy were more likely to have a mood disorder or experience incontinence. Some reported that epilepsy resulted in negative interactions with others, sleep interference, and educational, employment and driving limitations. On the other hand, 39% felt that overall their life was not impacted. Some reported out-of-pocket medication expenses and side effects, but most (90%) of those who felt better than when they had first been diagnosed credited medication for the improvement.
Acknowledgments
Statistics Canada thanks all participants for their input and advice during the development of the neurological content for the Canadian Community Health Survey, the Survey on Living with Neurological Conditions in Canada, and the Survey of Neurological Conditions in Institutions in Canada. The content of these surveys was developed jointly by the Health Statistics Division at Statistics Canada and the Public Health Agency of Canada (PHAC), with input from PHAC’s expert advisory group members who specialize in the study of neurological conditions. Content was selected based on objectives and data requirements specified by PHAC. Sponsorship was provided by PHAC as part of the National Population Health Study of Neurological Conditions.
Data source
This study is based on cross-sectional, nationally representative data from the 2011 Canadian Community Health Survey (CCHS) (63,542 respondents; response rate 69.8%); the Neurological Conditions Prevalence File (285,971 respondents; response rate 70.6%), derived from the 2010 and 2011 CCHS; the 2011 Survey on Living with Neurological Conditions in Canada (SLNCC) (4,569 respondents; response rate 81.6%); and the 2011/2012 Survey of Neurological Conditions in Institutions in Canada (SNCIC) (4,245 institutions; response rate 63.5%). These surveys are described in previous studies.
The analysis of people aged 15 or older in the household population with epilepsy was based on a sample of 714 respondents (305 men, 409 women).
Definitions
Respondents were asked about selected chronic neurological conditions (including epilepsy) that had lasted or were expected to last six months or more and had been diagnosed by a health professional.
Other self-reported chronic conditions were: bladder and/or bowel incontinence, high blood pressure (with related medication in the past month), heart disease, diabetes (except during pregnancy), and mood disorder.
Respondents were asked, “Overall, how much do you feel that your neurological condition(s) affects your life?” Responses were grouped as “not at all,” “a little bit/moderately,” and “quite a bit/extremely.”
Respondents with neurological conditions were asked four questions about social interactions. Those who responded “always” or “often” versus “sometimes,” “rarely” or “never” were considered to have interactions that had been affected by the condition.
Respondents older than 16 with a valid driver’s license were asked if their neurological condition had ever prevented them from driving.
Answers to the question, “How much do you feel that your condition has limited you in getting a good night’s sleep?” were grouped as “not at all” versus “a little bit/moderately/quite a bit/extremely.”
Separate questions addressed the extent to which the condition limited educational and job opportunities. Responses were grouped as “not at all,” “a little bit/moderately” or “quite a bit/extremely.”
Based on their employment status in the week before the interview, respondents 75 or younger were classified as currently working if they had worked at a job or business or had been absent from work; not currently working; or permanently unable to work.
“Changed work activities” indicates whether respondents who had previously been employed had ever changed their work activities (reduced hours, changed type of work, or stopped work altogether) for at least three months because of their neurological condition.
Respondents were asked to estimate their out-of-pocket spending over the past 12 months on prescription and non-prescription medications. These were expenses that would not be reimbursed by insurance or government programs. Responses were categorized as less than $500 versus $500 or more.
Those who reported side effects from the medications were asked how much the side effects affected their life (“not at all/a little bit” versus “moderately/quite a bit/extremely”).
Responses to the question “Compared to when you first diagnosed, how you would say your epilepsy is now?” were grouped as “much/somewhat better” versus “the same/somewhat or much worse.” Selected reasons for improvement were medication, coping strategies, and surgery.
Analysis
Weighted frequencies, cross-tabulations and means were calculated to examine the prevalence of epilepsy and its impact. To account for survey design effects, standard errors and coefficients of variation were estimated using the bootstrap technique. Prevalence estimates for the household and institutional populations were calculated for each survey separately and then combined, as per the separate approach to estimation. Confidence intervals for the combined estimate were calculated using the pooled variance technique. While it is possible that an individual could have been included in both surveys, the likelihood was judged to be small, and the surveys were treated as independent. The effect on the combined estimate of different methods of ascertaining epilepsy status between the household (self-report) and institutional (administration report) surveys is not known.
Estimates with a coefficient of variation of 16.6% to 33.3% are designated with a superscript E.
Limitations
The prevalence of neurological conditions was based on self-reported diagnosis by individual or proxy respondents for the household survey, and in aggregate by administrative staff for institutions, and not verified by any other source. It is not known if this under- or overestimates prevalence. For institutions, only prevalence data were available; therefore, most analyses concern the household population and do not represent residents of long-term residential care facilities. Detailed analysis of people with epilepsy in the household population (based on the SLNCC) is restricted to those aged 15 or older.
Inconsistencies emerged between the CCHS and the SLNCC in the respondents identified as having epilepsy: 105 respondents who had epilepsy in the CCHS did not in the SLNCC; 48 who had epilepsy in the SLNCC did not in the CCHS. This may have been due to differences in how people responded in each survey or eligibility for the surveys based on screening questions. Details are available elsewhere.